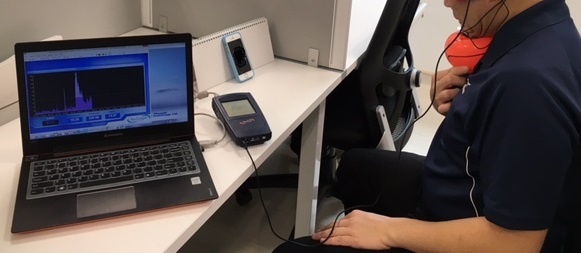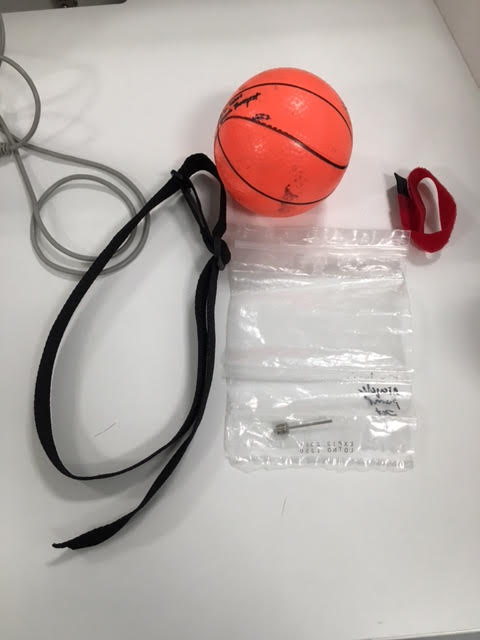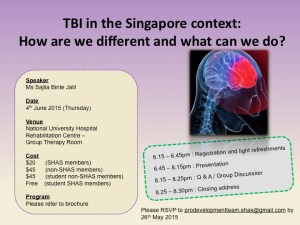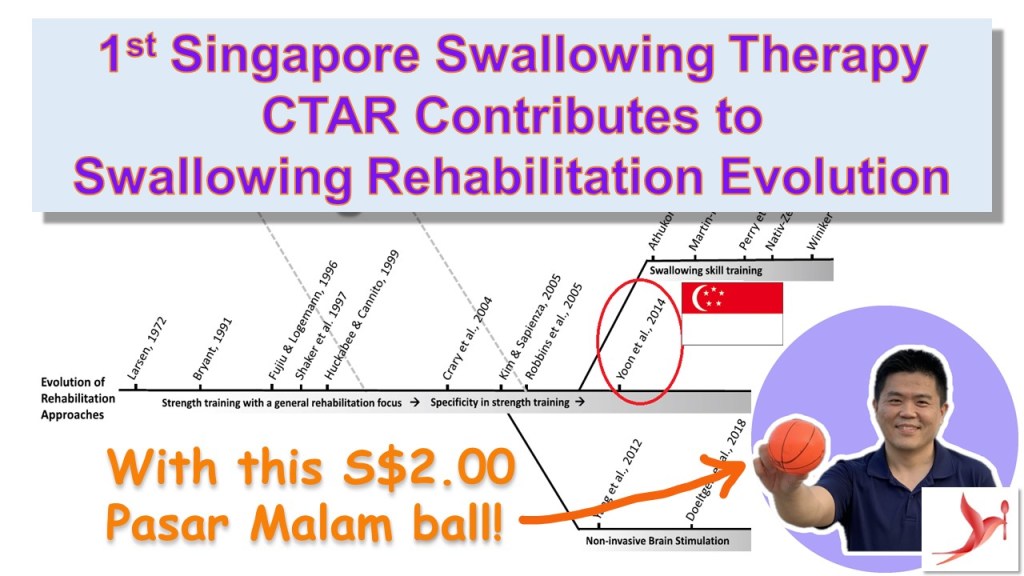
The year 2023 marks a monumental achievement for the Singapore Speech Therapy/Dysphagia community as CTAR (Chin Tuck Against Resistance), the inaugural swallowing therapy exercise, gains recognition for its pivotal role in advancing swallowing rehabilitation (Huckabee et al., 2023). Invented by Mr. Yoon Wai Lam, a distinguished Speech Therapist from Singapore, CTAR aims to provide a simple, economical, and highly effective exercise for strengthening the suprahyoid muscles involved in swallowing. Mr. Yoon first developed CTAR using a S$2.00 ‘pasar malam’ (a Malay word meaning night market in Singapore) inflatable rubber ball.
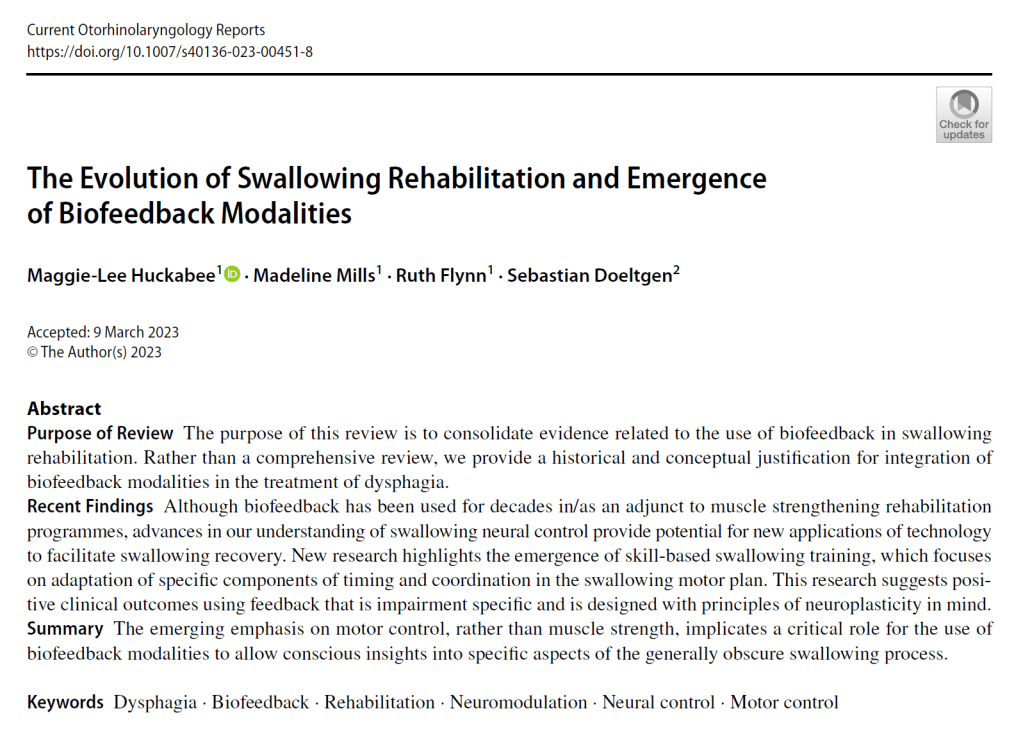
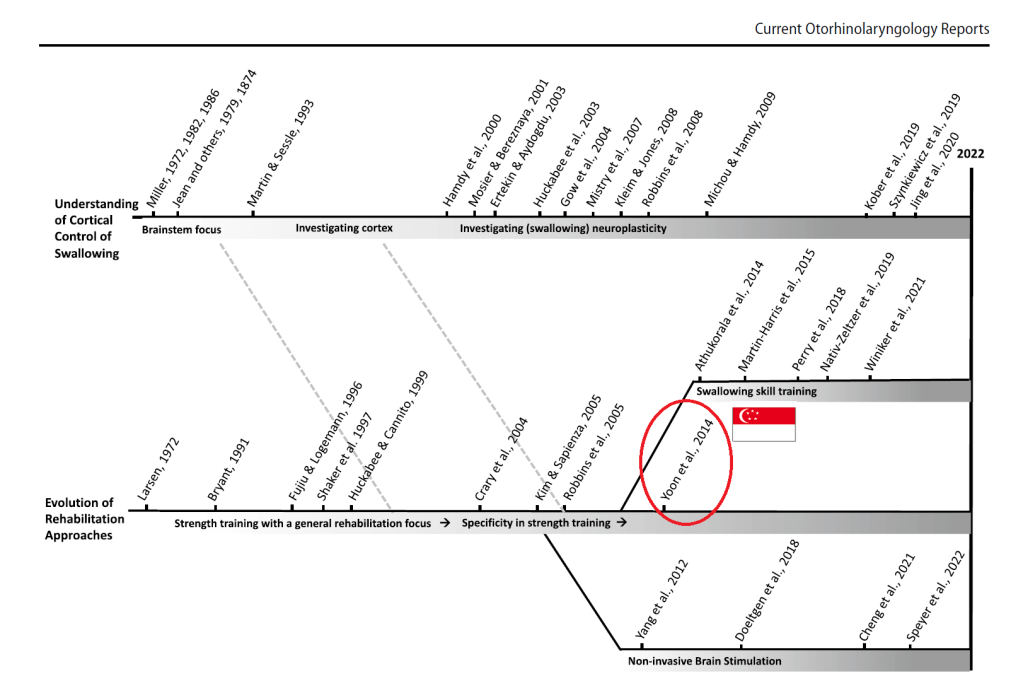
Huckabee, ML., Mills, M., Flynn, R. et al. The Evolution of Swallowing Rehabilitation and Emergence of Biofeedback Modalities. Curr Otorhinolaryngol Rep 11, 144–153 (2023). https://doi.org/10.1007/s40136-023-00451-8
CTAR made its global debut at the Dysphagia Research Society conference in 2013 in Seattle, Washington, USA. The unexpected surge of interest and the honor of receiving first place for the Scientific Abstract Poster underscored CTAR’s immediate impact. The initial CTAR journal article, published in Dysphagia Journal in 2014, quickly became one of the top 10 most downloaded articles of that year. A subsequent 2016 article further solidified its influence, collectively amassing 157 citations in various textbooks and journal articles to date.
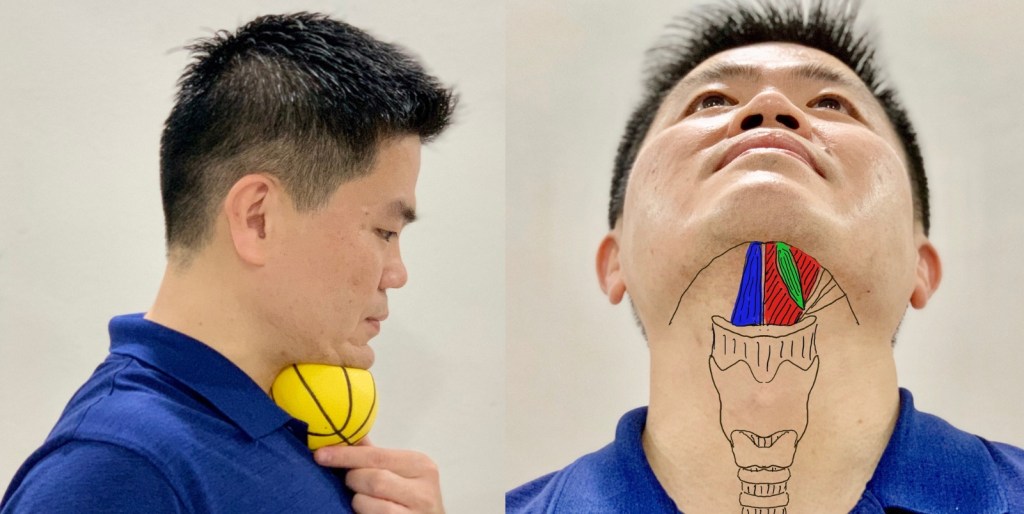
Beyond its original conception, CTAR inspired the development of numerous devices globally. However, Mr. Yoon distinguished himself by advancing the CTAR procedure without additional costs or commercial devices, relying solely on hand movements.
In a commendable move towards accessibility, Mr. Yoon launched the Singapore Swallowing Specialists YouTube Channel (http://www.youtube.com/@singaporeswallowingspecial735). This platform provides free CTAR videos in multiple languages, reaching over 60 thousand individuals worldwide.
The details of the CTAR exercise can be found at the following links:
- https://dysphagia.sg/2020/05/31/dysphagia-swallowing-therapy-chin-tuck-against-resistance-ctar-with-rubber-ball/
- https://dysphagia.sg/ctar-research/ctar-research/
References:
- Huckabee, ML., Mills, M., Flynn, R. et al. The Evolution of Swallowing Rehabilitation and Emergence of Biofeedback Modalities. Curr Otorhinolaryngol Rep 11, 144–153 (2023). https://doi.org/10.1007/s40136-023-00451-8
- Sze, W. P., Yoon, W. L., Escoffier, N., & Rickard Liow, S. J. (2016). Evaluating the Training Effects of Two Swallowing Rehabilitation Therapies Using Surface Electromyography-Chin Tuck Against Resistance (CTAR) Exercise and the Shaker Exercise. Dysphagia, 31(2), 195–205. http://doi.org/10.1007/s00455-015-9678-2
- Yoon, W.L., Khoo, J., & Liow, S. (2014). Chin tuck against resistance (CTAR): a new method for enhancing suprahyoid muscle activity using a Shaker-type exercise. Dysphagia. Retrieved from http://link.springer.com/article/10.1007/s00455-013-9502-9